Is it Ethical to Utilize the MyoVision for Public Screenings to Determine Potential Spinal Disorders?
By David Marcarian, MA
NIH Principal Investigator, Former NASA Researcher
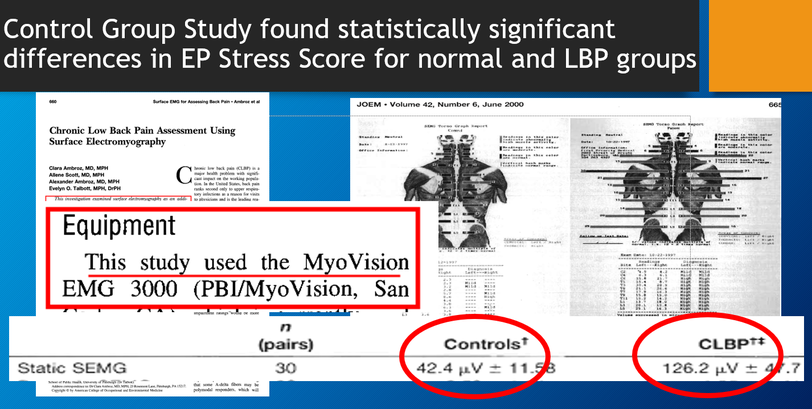
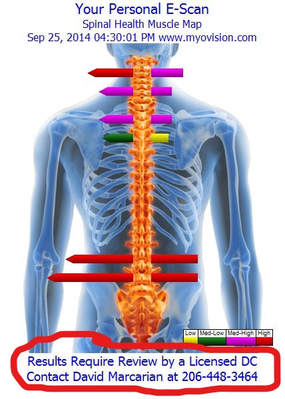
First of all, what is the MyoVision? It’s a static sEMG scanner. It’s very likely that you have a negative point of view on sEMG, as it does have a rather dubious history. I can confidently say, with the support of the VA Hospital, , the MyoVision is not like other sEMG scanners, which are plagued with a history of technical issues. The MyoVision device is a very sensitive, accurate form of electronic palpation; it precisely measures the body’s natural defense mechanism to pain: muscle guarding and splinting. The levels of muscle activity are demonstrated with the length and color of the bars. They are proportional to levels of muscle tension, with arrows pointing in the direction of imbalance. Red readings are high, magenta moderate and yellow are low. Both low and high readings are important as red indicates very high levels of muscle guarding, and yellow indicates potentially chronic levels of muscle tension.
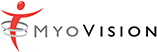
The MyoVision system is a Class II diagnostic device, which has been used in VA Hospital studies and directly called “the most advanced type of equipment” by researchers at the VA. It has been tested in control group studies and published in peer reviewed journals, and is the only device of its kind with this distinction. It’s also safer than most regulary used medical devices, like full body scans and X-Ray, where damaging radiation can negatively impact health. The MyoVision scanner is so harmless, it can be used on pregnant women, children and even on those with pacemakers. It is simply a measuring device with no radiation of any kind.
I, David Marcarian, am the designer of The MyoVision. It was designed under a National Institutes of Health Grant (NIH) after I completed my research work at NASA. As the designer of the device, I am the first to criticize those using it inappropriately. I have authored the paper, “A proposed quality assurance program for the clinical use Surface Electromyography in the chiropractic office,” published in the Journal of the Canadian Chiropractic Association and am well qualified to discuss the issues associated with public screenings and the use of sEMG technology. Healthcare practitioners who distort the MyoVision data to deceive the public into purchasing care plans not only damages my credibility, but my invention as well. I do not believe misrepresenting science to trick the public into chiropractic care has any benefit to the chiropractic profession. There is a legitimate and valuable application of Surface EMG technology in the screening setting when used properly, and when the results are presented accurately without embellishment.
I once testified against a chiropractor who claimed the Static sEMG results proved the patient would eventually develop cancer if they were not adjusted. My testimony led to the loss of their license.
I have over 30 years’ experience working with Surface EMG, and have run into 3 cases where the pattern of muscle activity was so unusual, I sent the patient for further analysis to evaluate issues with kidneys, liver and spleen – two of the three cases having undiagnosed cancer. In other words, the Static sEMG DOES have incredible value, as extremely unusual patterns of muscle firing are indicative of some underlying cause. The Static sEMG provided the clue that lead to appropriate treatment and ultimately saved their lives. But it was never presented as proof of need for any particular treatment in these 3 cases. Mechanical sources of back pain are much easier to tie to the MyoVision Static sEMG results.
Screening is so well accepted that almost every pharmacy has an automated blood pressure cuff. We’ve all seen it and likely used it. Though it has limited capability in the pharmacy setting, it does allow patients to educate themselves on the status of their blood pressure. Those results may compel them to make an appointment with their doctor who will perform a full evaluation and determine whether there is a true medical issue or not. Well being comes from awareness, and that is the purpose of using this device.
The Department of Health and Human Services (HHS) recommends screening for health issues on their website. Why? Preventative care. If we seek out solutions to ailments before they become serious, it will lower the cost of healthcare and improve everyone’s quality of life.
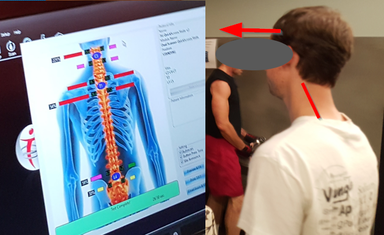
In the case shown in the photo below, the information provided by the Static sEMG was life changing. This patient had severe head forward position and the data from his sEMG scan led him to see a chiropractor. This chiropractor not only adjusted him, but also reminded him about the importance of proper ergonomics. He was working with a laptop, looking down with his hands lifted up on the table. She told him to get an external monitor so he could look up and a keyboard drawer with external keyboard so he could get his elbows at a 90 degree angle. Head forward position was demonstrated so clearly in the high levels of muscle tension in his upper thoracic (the upper thoracic is what compensates for the head being placed forward), that this objective data led to him fixing the problem and a long-term solution including not only chiropractic care but proper ergonomics. A win-win-win for everyone.
When the Clinic Director at Palmer College in Florida, who has 20 years experience using the MyoVision, was asked if there was anything illegal or unethical about Palmer Florida performing public screenings with the MyoVision Static sEMG, he responded, “As long as HIPAA and confidentiality is maintained, a sample screening would not lead to a diagnosis without a full history and exam, and that would be performed in office.”
To further confirm this, he checked with the State Board’s attorney who put in writing:
“There are no issues as long as PHI was protected and the DC offering it for free had a disclaimer with full price noted of the free service and did not attempt to rescreen at the office and submit a bill or charge for the service.”
When it comes right down to it, any test, no matter who performs it, can be abused, misused or misrepresented. So, is there a way to avoid this? Yes, with proper education and knowledge. This idea is being implemented throughout the country in chiropractic colleges.
Many Chiropractic Colleges now routinely screen with the MyoVision, but require that each screener complete the online certification course so they 1) perform the test properly, and 2) know what is appropriate to say when interpreting the results. This online certification course is required by Palmer College, Life Chiropractic College West, University of Western States and Life University prior to using at any screening. By properly training at the beginning, we have begun to resolve the matter of individuals lacking the knowledge of proper utilization, limitations and explanation of the results. My recommmendations with regards to quality control and screening in public: Education is critical. The chiropractic colleges have approved the Online Certification Course, and anyone performing a screening should have proof of completing.
To summarize:
 Everyone performing the test must complete the online certification course, which is approved by the chiropractic colleges. This will ensure proper test technique, so false positives and negatives are reduced.
Everyone performing the test must complete the online certification course, which is approved by the chiropractic colleges. This will ensure proper test technique, so false positives and negatives are reduced.- Screeners must never present the data with diagnosis. They should explain the results provide a quick screening to show their particular muscular compensation for their bio-mechanical issues, which lack the clinical accuracy of a test performed in the office.
- A disclaimer (shown to the right) can be used to make certain there is no questions with regards to the statements made during the screening. This is a patented process that embeds this text into the graphic so it cannot be altered. This may be used as a requirement at all screenings to prevent miscommunication.
With the advent of technology to improve preventative care, every specialty in medicine has a form of screening tool implemented. Medical doctors have blood pressure cuffs in pharmacies, full body scans are being offered by many clinics, and even cardiac screenings are being done for arterial plaque. These screenings are never definitive, but are used as a detective uses data: To develop a clue as to the source of underlying potential health risks, so they can be addressed preemptively, and result in long-term health. The situation is no different with chiropractic: Chiropractors are licensed practitioners, and the MyoVision has been selected as the Gold Standard by both the AMA, the VA and most of the Chiropractic Colleges meaning that it’s use by Doctors as a screening tool is completely legitimate. Just like the MD reading an MRI, it is simply important that the Chiropractor not misrepresent the results. That being the case, the number of patients helped through this tool which makes them aware of their spinal health, and potential biomechanical issues is crucial to a system based upon patient-centered care, as the MyoVision puts the patient’s spine in the center of the discussion.
REFERENCES
- Geisser ME, Wiggert EA, Haig AJ, Colwell MO. A randomized, controlled trial of manual therapy and specific adjuvant exercise for chronic low back pain. Clin J Pain (in press).
- Rosomoff HL, Fishbain DA, Goldberg M, Santana R, Rosomoff RS. Physical findings in patients with chronic intractable benign pain of the neck and/or back. Pain 1989; 37: 279-87.
- Gatchel RJ, Polatin PB, Kinney RK. Predicting outcome of chronic back pain using clinical predictors of psychopathology: a prospective analysis. Hlth Psychol 1995;14:415-20.
- Gatchel RJ, Polatin PB, Mayer TG. The dominant role of psychosocial risk factors in the development of chronic low back pain disability. Spine 1995;20:2702-9.
- Cram JR, Steger JC. EMG scanning in the diagnosis of chronic pain. Biofeedback and Self-Regulation 1983;8:229-41.
- Dolce JJ, Raczynski JM. Neuromuscular activity and electromyography in painful backs: Psychological and biomechanical models in assessment and treatment. Psychol Bull 1985;97:502-20.
- Greenman PE. Syndromes of the lumbar spine, pelvis and sacrum. Phys Med Rehabil Clin North Amer 1996;7:773-85.
- Mense S. Nociception from skeletal muscle in relation to clinical pain. Pain 1993;54:241-89.
- Watson PJ, Booker CK, Main CJ, Chen AC. Surface electromyography in the identification of chronic low back pain patients: the development of the flexion relaxation ratio. Clin Biomech 1997;12:165-71.
- Ohrbach R, McCall WD Jr. The stress-hyperactivity-pain theory of myogenic pain. Pain Forum 1996;5:51-66.
- Cobb CR, deVries HA, Urban RT, Luekens CA, Bagg RJ. Electrical activity in muscle pain. Amer J Phys Med 1975;54:80-7.
- Nouwen A, Bush C. The relationship between paraspinal EMG and chronic low back pain. Pain 1984;20:109-23.
- Haig AJ, Gelblum JB, Rechtein JJ, Gitter AJ. Technology assessment: the use of surface EMG in the diagnosis and treatment of nerve and muscle disorders. Muscle Nerve 1996;19:392-5.
- Pullman SL, Goodin DS, Marquinez AI, Tabbal S, Rubin M. Clinical utility of surface EMG. Report of the Therapeutics and Technology Assessment subcommittee of the American Academy of Neurology. Neurol 2000;55:171-7.
- Dumitru D. Practical aspect of instrumentation. In: Johnson EW, Pease WS (eds), Practical electromyography (3rd ed.). Baltimore: Williams & Wilkins, 1997:63-87.
- Mayer TG, Kondraske G, Mooney V, Carmichael TW, Butsch R. Lumbar myoelectric spectral analysis for endurance assessment. A comparison of normals with deconditioned patients. Spine 1989;14:986-91.
- Wolf SL, Nacht M, Kelly JL. EMG feedback training during dynamic movement for low back pain patients. Behav Ther 1982;13:395-406.
- Haig AJ, Weismann G, Haugh LD, Pope M, Grobler LJ. Prospective evidence for change in paraspinal muscle activity after herniated nucleus pulposus. Spine 1993;18:926-30.
- Crombez G, Vlaeyen JWS, Heuts PHTG, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain 1999;80:329-339.
- Flor H, Birbaumer N, Turk DC. The psychobiology of chronic pain. Adv Behav Res Ther 1990;12:47-84.
- Geisser ME, Haig AJ, Wallbom AS, Wiggert EA. Pain-related fear, lumbar flexion, and dynamic EMG among persons with chronic musculoskeletal low back pain. Clin J Pain 2004;20:61-69.
- Robinson ME, Riley JL 3rd. Models of pain. In: Block AR, Kremer EF, Fernandez E (eds), Handbook of pain syndromes: biopsychosocial perspectives. Mahwah NJ: Lawrence Erlbaum, 1998:23-40.
- Elert J, Kendall SA, Larsson B, Mansson B, Gerdle B. Chronic pain and difficulty in relaxing postural muscles in patients with fibromyalgia and chronic whiplash associated disorders. J Rheumatol 2001;28:1361-8.
- Nederhand MJ, IJzerman MJ, Hermens HJ, Baten CT, Zilvold G. Cervical muscle dysfunction in the chronic whiplash associated disorder grade II (WAD-II). Spine 2000 Aug 1;25(15):1938-43.
- Cohen J. Statistical power analysis for the behavioral sciences, 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates, 1988.
- Chen WJ, Chiou WK, Lee YH, Lee MY, Chen ML. Myo-electric behavior of the trunk muscles during static load holding in healthy subjects and low back pain patients. Clin Biomech 1998;13(Suppl):S9-S15 .
- Chiou W-K, Lee Y-H, Chen W-J.Use of the surface EMG coactivational pattern for functional evaluation of trunk muscles in subjects with and without low-back pain. Int J Ind Ergon 1999;23:51-60.
- Collins GA, Cohen MJ, Naliboff BD, Schandler SL. Comparative analysis of paraspinal and frontalis EMG, heart rate and skin conductance in chronic low back pain patients and normals to various postures and stress. Scand J Rehabil Med 1982;14:39-46.
- Hubley-Kozey CL, Vezina MJ. Differentiating temporal electromyographic waveforms between those with chronic low back pain and healthy controls. Clin Biomech 2002;17:621-9.
- Kramer M, Katzmaier P, Eisele R, Ebert V, Kinzl L, Hartwig E. Surface electromyography-verified muscular damage associated with the open dorsal approach to the lumbar spine. Eur Spine J 2001;10:414-20.
- Leach RA, Owens EF Jr, Giesen JM. Correlates of myoelectric asymmetry detected in low back pain patients using hand-held post-style surface electromyography. J Manipulative Physiol Ther 1993;16:140-9.
- Mooney V, Gulick J, Perlman M, Levy D, Pozos R, Leggett S, Resnick D. Relationships between myoelectric activity, strength, and MRI of lumbar extensor muscles in back pain patients and normal subjects. J Spinal Disord 1997;10:348-56.
- Newcomer KL, Jacobson TD, Gabriel DA, Larson DR, Brey RH, An K. Muscle activation patterns in subjects with and without low back pain. Arch Phys Med Rehabil 2002;83:816-21.
- Oddsson LI, Giphart JE, Buijs RJ, Roy SH, Taylor HP, De Luca CJ. Development of new protocols and analysis procedures for the assessment of LBP by surface EMG techniques. J Rehabil Res Dev 1997;34:415-26.
- Pope MH, Aleksiev A, Panagiotacopulos ND, Lee JS, Wilder DG, Friesen K, Stielau W, Goel VK. Evaluation of low back muscle surface EMG signals using wavelets. Clin Biomech 2000;15:567-73.
- Rosenthal R. Writing meta-analytic reviews. Psychol Bull 1995;118:183-92.
- Hedges LV. Distribution theory for Glass’s estimator of effect sizes and related estimators. J Educ Statistics 1981;6:107-28.
- Ahern DK, Follick MJ, Council JR, Laser-Wolston N, Litchman H. Comparison of lumbar paravertebral EMG patterns in chronic low back pain patients and non-pain controls. Pain 1988;34:153-60.
- Ambroz C, Scott A, Ambroz A, Talbott EO. Chronic low back pain assessment using surface electromyography. J Occup Environ Med 2000;42:660-9.
- Arena JG, Sherman RA, Bruno GM, Young TR. Electromyographic recordings of 5 types of low back pain subjects and non-pain controls in different positions. Pain 1989;37:57-65.
- Arena JG, Sherman RA, Bruno GM, Young TR. Temporal stability of paraspinal electromyographic recordings in low back pain and non-pain subjects. Int J Psychophysiol 1990;9:31-7.
- Arena JG, Sherman RA, Bruno GM, Young TR. Electromyographic recordings of low back pain subjects and non-pain controls in six different positions: effect of pain levels. Pain 1991;45:23-8.
- DeGood DE, Stewart WR, Adams LE, Dale JA. Paraspinal EMG and autonomic reactivity of patients with back pain and controls to personally relevant stress. Percept Mot Skills 1994;79:1399-409.
- Jalovaara P, Niinimäki T, Vanharanta H. Pocket-size, portable surface EMG device in the differentiation of low back pain patients. Eur Spine J 1995;4:210-2.
- Lofland KR, Cassisi JE, Levin JB, Palumbo NL, Blonsky ER. The incremental validity of lumbar surface EMG, behavioral observation, and a symptom checklist in the assessment of patients with chronic low-back pain. Appl Psychophysiol Biofeedback 2000;25:67-78.
- Miller DJ. Comparison of electromyographic activity in the lumbar paraspinal muscles of subjects with and without chronic low back pain. Phys Ther 1985;65:1347-54.
- Ng JK-F, Richardson CA, Parnianpour M, Kippers V. EMG activity of trunk muscles and torque output during isometric axial rotation exertion : a comparison between back pain patients and matched controls. J Orthop Res 2002 ; 20:112-121.
- Shirado O, Ito T, Kaneda K, Strax T. Flexion-relaxation phenomenon in the back muscles: a comparative study between healthy subjects and patients with chronic low back pain. Am J Phys Med Rehabil 1995;74:139-44.
- Sihvonen T, Partanen J, Hänninen O, Soimakallio S. Electric behavior of low back muscles during lumbar pelvic rhythm in low back pain patients and healthy controls. Arch Phys Med Rehabil 1991;72:1080-7.
- Sihvonen T, Huttunen M, Makkonen M, Airaksinen O. Functional changes in back muscle activity correlate with pain intensity and prediction of low back pain during pregnancy. Arch Phys Med Rehabil 1998;79:1210-2.
- Alexiev AR. Some differences of the electromyographic erector spinae activity between normal subjects and low back pain patients during the generation of isometric trunk torque. Electromyogr Clin Neurophysiol 1994;34:495-9.
- Capodaglio P, Nilsson J. Functional correlates in the rehabilitation of occupational low back pain. G Ital Med Lav 1996;18:35-9.
- Cassisi JE, Robinson ME, O’Connor P, MacMillian M. Trunk strength and lumbar paraspinal muscle activity during isometric exercise in chronic low-back pain patients and controls. Spine 1993;18:245-51.
- Elfving B, Dedering A, Németh G. Lumber muscle fatigue and recovery in patients with long-term back trouble – electromyography and health-related factors. Clin Biomech 2003;18:619-30.
- Kankaanpää M, Taimela S, Laaksonen D, Hannien O, Airksinen O. Back and hip extensor fatigability in chronic low back pain patients and controls. Arch Phys Med Rehabil 1998;79:412-7.
- Lee DJ, Stokes MJ, Taylor RJ, Cooper RG. Electro and acoustic myography for noninvasive assessment of lumbar paraspinal muscle function. Eur J Appl Physiol Occup Physiol 1992;64:199-203.
- Lisiński P. Surface EMG in chronic low back pain. Eur Spine J 2000;9:559-62.
- Lu WW, Luk KD, Cheung KM, Wong YW, Leong JC. Back muscle contraction patterns of patients with low back pain before and after rehabilitation treatment: an electromyographic evaluation. J Spinal Disord 2001;14:277-82.
- Pääsuke M, Johanson E, Proosa M, Ereline J, Gapeyeva H. Back extensor muscle fatigability in chronic low back pain patients and controls: Relationship between electromyogram power spectrum changes and body mass index. J Back Musculoskeletal Rehabil 2002;16:17-24.
- Peach JP, McGill SM. Classification of low back pain with the use of spectral electromyogram parameters. Spine 1998;23:1117-23.
- Robinson ME, Cassisi JE, O’Connor PD, MacMillian M. Lumbar iEMG During Isotonic Exercise : Chronic Low Back Pain Patients Versus Controls. J Spinal Disord 1992;5:8-15.
- Roy SH, De Luca CJ, Casavant DA. Lumbar muscle fatigue and chronic lower back pain. Spine 1989;14:992-1001.
- Suter E, Lindsay D. Back muscle fatigability is associated with knee extensor inhibition in subjects with low back pain. Spine 2001;26:E361-6.
- Klein AB, Snyder-Mackler L, Roy SH, DeLuca CJ. Comparison of spinal mobility and isometric trunk extensor forces with electromyographic spectral analysis in identifying low back pain. Phys Ther 1991;71:445-54.
- Roy SH, De Luca CJ, Snyder-Mackler L, Emley MS, Crenshaw RL, Lyons JP.
- Roy SH, De Luca CJ, Emley M, Buijs RJ. Spectral electromyographic assessment of back muscles in patients with low back pain undergoing rehabilitation. Spine 1995;20:38-48.
- Radebold A, Cholewicki J, Panjabi M, Patel T. Muscle response pattern to sudden trunk loading in healthy individuals and in patients with chronic low back pain. Spine 2000;25:947-54.
- Radebold A, Cholewicki J, Polzhofer GK, Greene HS. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine 2001;26:724-30.
- Leinonen V, Kankaanpää M, Luukkonen M, Hänninen O, Airaksinen O, Taimela S. Disc herniation-related back pain impairs feed-forward control of paraspinal muscles. Spine 2001;26:E367-72.
- Neblett R, Mayer TG, Gatchel RJ, Keeley J, Proctor T, Anagnostis C. Quantifying the lumbar flexion-relaxation phenomenon. Theory, normative data, and clinical applications. Spine 2003;28:1435-46.
- Geisser, ME, Ranavaya, M, Haig, AJ, Roth, RS, Zucker, R., Ambroz, C, Caruso, M. A meta-analytic review of surface EMG among persons with low back pain and normal, healthy controls. The Journal of Pain, Vol 6, No 11 (November) 2005: pp 711-726.
- Gerhardt, JJ, Cocchiarella , L & Lea, R.A. The Practical Guide to Range of Motion Assessment, 2009.
- Motion Assessment, 2009. Published by the American Medical Association.
- Merritt vs. Florida DOH. Case # 04-1149RX Download case files at https://www.dynarom.com/supreme-court-case.html
- King County Superior Case # 16-2 29568-1 SEA